Автор: http://www.newsweek.com/
When 40-year-old Liberian civil servant Patrick Sawyer died of Ebola earlier this year in hospital in Lagos, having carried the disease from his home country to Nigeria, global health workers feared the epidemic would spread in West Africa’s most populous city. But no one paid much attention to the victim of another epidemic further north.
One day before Sawyer’s death, on 24 July, the worried parents of a 16-month-old toddler in Kano state had discovered their child was suffering from the symptoms of a disease had supposedly been largely wiped out of existence – poliomyelitis.
Although the two viruses are very different, the efforts to tackle polio and Ebola have been intricately connected, largely through the efforts of the 30 year, multi-billion dollar, global polio eradication campaign that stands on the brink of wiping out polio – but that brink is precarious. If the teams involved succeed, global disease eradication will have a new blue-print. The consequences of not succeeding – after decades of painstaking work across the world – seem impossible to contemplate.
Polio has been almost entirely extinguished from the collective memory of anyone living in Europe or the US. It’s taken $8.6bn (£5.5bn) to achieve 99% eradication of polio and it’s going to cost an estimated further $4.5bn to tackle the remaining 1% of cases during the next four years.
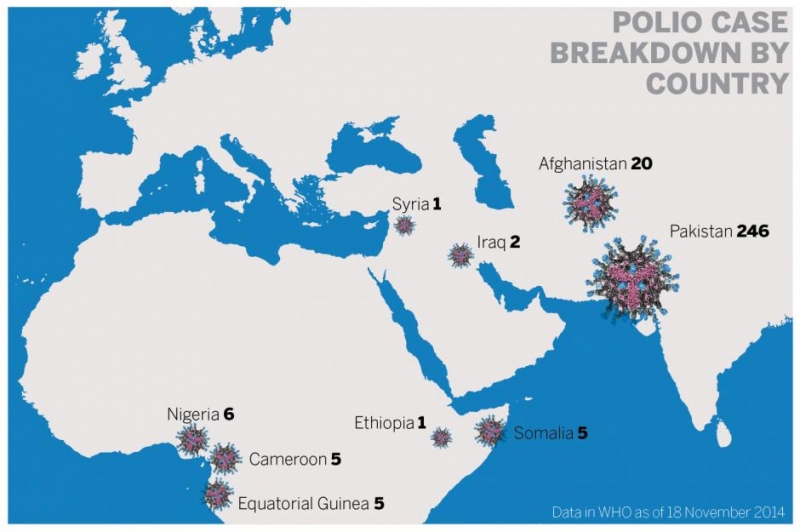
Earlier this month Dr Stephen Cochi of the CDC’s Centre for Global Health announced a “major milestone” with the likely elimination of the second of the three strains of the wild polio virus (subject to a surveillance period of three years). But internationally, war and insecurity makes wiping out polio’s tiny number of remaining cases frustratingly elusive. In March 2014, the World Health Organisation (WHO) admitted the scale of the problem, announcing: “The fight to eliminate polio is now imperiled . . . by insecurity, targeted attacks on health workers and/or a ban by local authorities on polio immunisation.” The final stage of the fight against polio is hanging in the balance. Not only must workers target endemic areas of Pakistan, Afghanistan and Nigeria, where polio has never been wiped out – they must also access war zones in Syria, Somalia, Iraq and across the Horn of Africa where polio has returned in areas of conflict, making it impossible for vaccinators to work.
Those involved fear their work will simply have given satisfaction to critics of the long campaign who claim it has spent a bottomless pit of money and effort chasing an impossible dream – money and effort that could have been better spent on more achievable health efforts around the world.
No-one feels that pressure more keenly than doctor Faisal Shuaib. Despite the fact that Nigeria is officially Ebola-free as a direct result of his own work against polio, the death of another child from polio hits his team hard.
Faisal grew up in northern Nigeria and, after qualifying as a doctor, took up a position in public health for the WHO, becoming deputy incident manager at Nigeria’s innovative polio Emergency Operations Centre (EOC). When Nigeria’s first Ebola case was diagnosed, he was immediately transferred to head up an Ebola EOC.
For Shuaib, the polio diagnosis of 24 July was tough moment – the polio eradication campaign was within a whisper of a phenomenal breakthrough, but yet another child was paralysed after missing some of the repeated series of immunisations so important in tackling the virus in areas with poor sanitation. “I grew up seeing people crippled by polio along the sides of the road,” Shuaib says, “Eradication is within reach and we are on the cusp of Africa being polio free – but the gains we have made are fragile and we must not let the fight to tackle Ebola set the clock back.”
“The Ebola virus coming to Nigeria was something new, and its been tough,” Shuaib says. “Working on the polio programme is very demanding, but having to manage an Ebola outbreak of this magnitude has meant living with the possibility that if you don’t get it right it could have potentially overwhelmingly catastrophic consequences for the whole of West Africa. When you see your colleagues dying around you, it wears you down and saps all your faculties.”
Nonetheless, by implementing the same techniques that have proved so successful against polio – setting up an EOC to ensure a fast and co-ordinated response and establishing rapid house to house surveillance system – Shuaib and his colleagues appear to have brought the Ebola epidemic under their control in Nigeria.
THE FINAL HURDLE
The Nigerian response to both Ebola and polio is tracked and coordinated with a series of global health agencies, including the Center for Diseases Control and Prevention (CDC) in Atlanta, where a series of anodyne office buildings resemble a suburban office park rather than a high security complex that houses samples of the world’s deadliest diseases.
A walk to the polio lab at the CDC can involve passing the building that houses the last surviving stock of smallpox, riding on the lift past the floor where there was recently a leak from the anthrax lab, and turning the corner by the rabies lab, to find a test tube filled with a clear liquid, spinning frantically, ready to reveal whether it contains a variant of the polio virus transported overnight from an outbreak in East Africa.
Only 60 years ago, poliomyelitis conjured even greater terror than Ebola does today – striking silently, and without warning, across the world. The fact that it no longer inspires such fear is due in large part to the work of scientists like Dr Cara Burns, who runs the polio lab at the CDC. Together with the scientists and tacticians at CDC, a dedicated team at the WHO, UNICEF, Rotary International, and the billionaire philanthropy of Bill Gates, polio has been wiped out from 99% of the world.
“We can’t fail,” says Larry Brilliant, an epidemiologist and President of the Skoll Global Threats Fund, who played a key role in the successful WHO smallpox eradication program – the only other disease to have been totally eradicated. Despite the polio campaign’s breathtaking resources and technology (something it is reluctant to explain, as the campaign’s use of satellite mapping can be highly controversial in parts of the world), Brilliant sees the same spirit of idealism and endeavour that characterised the effort to eradicate smallpox 40 years earlier. “We must eradicate polio. And if we don’t it is not just this one disease and all of its human pain and suffering that’s at stake – it’s anything we might do in the future as a global health community.”
It is a campaign that used unprecedented resources in the battle; namely the most advanced satellite technology in the world to help map communities and track volunteers, combined with the oldest forms of transport, including canoes and camels, to transport vaccines – and a large element of human persuasion needed to win over politicians, religious leaders and parents into accepting the countless rounds of oral doses needed to make the vaccine successful. Each child must receive at least eight rounds.
It is also a campaign that many people are willing to risk their lives for. Polio vaccinators have been targeted and killed by rebel groups in Pakistan, Nigeria and the Horn of Africa. Since 2012, more than 50 polio volunteers and workers were murdered – more than are estimated to have died of polio.
THE POLIO BUSTERS
The lure of playing a part in what could be the biggest leap forward in global health in the 21st century seems irresistible, yet the hundred or so called polio-busters – health workers from 34 countries around the world who have gathered at the CDC in Atlanta for three weeks of intensive training before voluntary placements in the field – find it impossible to fully explain why that’s the case. Most will leave young families behind to undertake five months of unpaid placements delivering the polio vaccine. They know they are risking their lives.
Selamawit Satato, a quietly spoken 34-year-old nurse from the town of Soddo in Ethiopia, has recently volunteered to spend five months working as a polio volunteer in northern Nigeria where polio workers were targeted and killed in 2012, and where attacks by rebel groups like Boko Haram are a serious threat. “I feel I am in danger, she admits, “but I want to contribute to eradicating polio . . . and even if there is danger I have decided to go to Nigeria in order to put all my efforts into eradicating this disease.”
Impossible idealism, intense commitment, immense difficulty, internecine political negotiations, and sometimes bitter rivalry, have been the hallmarks of polio eradication from the very beginning. Polio was an unseen terror that stalked the early-to-mid 20th century; killing some, paralysing many more and bringing to mind horrific images of lives saved, but horribly restricted, in iron lungs where patients sometimes spent years unable to even drink a sip of water for themselves. At its height, 8,000 children were paralysed every year in the UK. By the 50s, however, polio appeared to be a disease of the past, with two competing (and acrimoniously contested) rival vaccines – the injected inactivated polio vaccine (IPV) developed by Jonas Salk, and the live oral polio vaccine (OPV) developed by Albert Sabin, dramatically reducing the number of cases. Urged on by populist campaigns initiated by the US government, the two men battled it out with their vaccines in an atmosphere of deep animosity.
When Salk’s vaccine was initially given widespread use in the United States, Sabin was forced to undertake his clinical trials in the Belgian Congo and Soviet Union. Vaccinating 10 million Soviet children at the height of the cold war earned Sabin a medal of gratitude from the Russian government – but tarred the OPV as the “red vaccine” for years to come. The success of early campaigns in communist states like Cuba, and then parts of central and South America, confirmed polio’s status as a curiously political disease – something that was dramatically heightened by the 2012 decision by factions of the Pakistan Taliban to ban vaccination in the North West tribal areas of Waziristan and Pakistan’s Khyber Pakhtunkhwa province after it was discovered that the CIA had instigated a fake door-to-door hepatitis B vaccination campaign in its efforts to locate Osama Bin Laden. The situation worsened when a Kathryn Bigelow film, Zero Dark Thirty, wrongly identified the doctor in charge of the campaign, Shakil Afridi, as a polio vaccinator. The ban quickly led to a ten-fold increase in polio cases (which had been as low as six the previous year) and the shocking murders of more than 60 polio workers in the course of two years. Similar claims that information gathered by the polio campaign is used for US spying is frequently given as justification for attacks on polio workers by rebel groups in other parts of the world too. “Polio has become a very, very political issue – rather than a humanitarian one,” says Sir Liam Donaldson, the former Chief Medical Officer of England who chairs the international monitoring board of the Global Polio Eradication Initiative (GPEI). “We need to move it back along the spectrum to becoming humanitarian again.”
VICTORY IN INDIA
“A whole life alters after you get polio,” says Hamid Jafari, Director of Global Polio Eradication and Research at the WHO and the man who oversaw the eradication of polio in India. “Jafari remembers treating his first polio patients in Punjab province in his native Pakistan. “Young mothers were coming to me with young infants who were paralysed, and those mothers had all of this hope in their eyes that maybe polio could be cured. They wanted me to treat their babies, but I knew they were looking at lifelong paralysis. That’s heart breaking, and that’s part of the inspiration and motivation that keeps you going.”
Although he now heads the team in Geneva, Jafari spent six years as Project Manager of the WHO’s National Polio Surveillance Project in India – working as the main technical advisor to the Indian government and managing 1,000 field staff. “India was the most polio endemic country for thousands of years, and in that context, because of its size, and because of its importance in the world, it was also a very important source of international spread of polio,” he says. The country struggled under a burden of up to 150,000 polio cases at a time, with population density, poor sanitation and climate making ideal conditions for the disease to thrive. “It took an extraordinary effort to achieve eradication in India.”
Цялата статия
http://www.newsweek.com/2014/12/05/last-stand-against-polio-287862.html